Andy the arm is what medical students use to practice taking blood before they go to try on real people! They can also practice placing cannulas and attaching intravenous (IV) fluids.
To take blood from Andy, first you must find a vein. In Andy, veins feel like squishy tubes, just under the skin. Then go in with the needle at an acute angle, with the hole at the end of the needle pointing upwards. Keep pushing the needle into Andy until you feel a slight nudge – this means you’re in the vein, so you can stop pushing the needle in, and start pulling the plunger up. If you got the vein then you should have some (fake!) blood in the syringe – well done!

Intubation is where you put a tube into a patient’s airways in order to help them breathe when they are unable to do this themselves. This is done in emergencies when patients are unconscious and unable to breathe or can be planned such as when someone is having anaesthetic for surgery.
Intubation is a tricky technique and requires lots of practice for student doctors to get this right. They practice on mannequins just like Eddy.
To insert a breathing tube into Eddy, first you have to lift his head up so that his airways are straightened – making them more accessible for the tube. Then, go in with the breathing tube, initially the wrong way up, then twist round once in the mouth and place. This is done so that you don’t knock the patient’s tongue down their throat. Once the tube is in position, you can then give Eddy some air by placing the mask over the airways and pumping the bag.

The lens of your eye focuses light through the clear liquid in your eye to the retina. The retina has special sensors on them that detect light and colour, and it turns this image into an electrical signal that is sent to the brain via the optic nerve. The brain then works to form one image from the signals sent from both eye – which is what you are seeing right now!
The pathology goggles show you what your vision would look like if you were a person with different eye problems – see below for what is which.
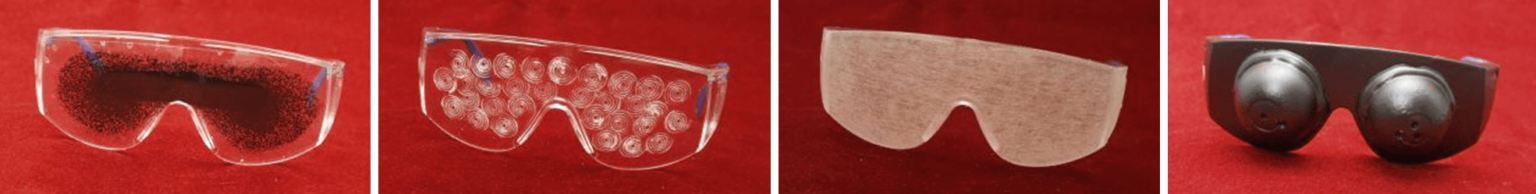
The ageing suit simulates the physical symptoms that elderly people can suffer with. Older people tend to suffer from stiff joints, bad balance, weaker eyesight and extra weight.
Why do we age? All the cells in your body are constantly being recycled – old ones are dying and are replaced with new ones. However, cells can only be replaced for a limited number of times and over time, as more cells are lost or damaged, more physical signs of ageing show.

There are lots of signs of ageing including:
A reflex hammer is used to test your tendon reflexes.
Tendons connect muscle to bone, usually over a joint. When the muscle contracts, the tendon pulls on the bone and causes movement.
When a tendon is hit by a reflex hammer, it sends impulses along nerves to the spinal cord to the motor neuron. The signal then goes back down the motor neuron to the target muscle which contracts and causes movement.
It is easiest to do this on your knee joint and should make your lower leg twitch. This test is done to check that your nerves and spinal cord are all working as they should, especially after trauma such as injuries or surgery which can damage the nerves.

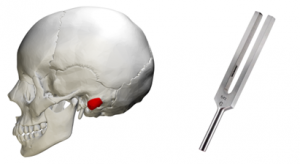
Tuning forks can be used to test your hearing. If a patient complains of hearing loss, these tests can find out where the problem is.
There are two types of test:
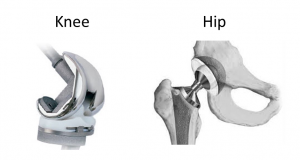
The joints in your body are constantly being used – over time these can wear away or can be damaged by diseases, such as arthritis, or injury. This can make the joints stiff and painful so the joint may need to be replaced.
Elderly people are most likely to need a joint replacement as they have worn joints and are more likely to have arthritis-like diseases. Joint replacements usually last around 15 years. Around 160,000 hip replacements are done in the UK every year.
The joint implant can be made of metal, ceramic, plastic or a combination of these materials. They are designed to be as much like the original joint as possible and to not wear too much.
Tuning forks can be used to test your hearing. If a patient complains of hearing loss, these tests can find out where the problem is.
There are two types of test:
We inspire the next generation of medics and scientists by taking real medical and sports science equipment into schools, colleges & events all over the UK.
Company: MedicFest Ltd, trading as Medical Mavericks. Registered in England and Wales. Company Number: 12021679
© 2024 Medical Mavericks. All rights reserved.